When Marilyn Cornelius woke up Aug. 16 with a stuffy nose, she thought she knew the cause.
“It was just after a particularly smoky weekend, so I figured it was the smoke,” the 56-year-old Sisters resident said.
But then she lost her sense of taste and smell, and Cornelius feared she had contracted COVID-19.
She was right.
“I went to get tested and that was the morning they were reopening drive-thru testing at St. Charles. They were literally setting up the tents when I arrived,” she said. “Sure enough, it came back positive, which was a bummer, because you try to do everything right but you still get nailed.”
Cornelius was vaccinated against COVID-19 in February, practices social distancing in public spaces and masks up when she feels she should. But by that night, she was isolated in her home, still not feeling terrible, but still without her senses of taste and smell.
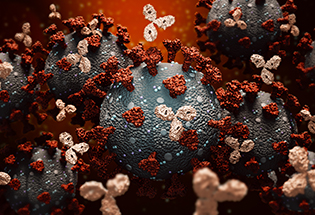
The next morning, Cornelius received an email informing her that she had a new message in MyChart. It was a chart note from St. Charles Family Care Dr. Carey Allen advising her that she qualified for monoclonal antibody (MAB) therapy, a treatment for people with mild-to-moderate symptoms of COVID-19 that helps keep people from getting sicker and having to be hospitalized.
“I immediately started Googling it and went, ‘Oh yeah, I want this,’” Cornelius said.
Since July, St. Charles has provided MAB therapy for more than 900 COVID-positive people. Among those, just 2% were eventually hospitalized, as compared to an 8% hospitalization rate for all COVID-positive patients at the health system. And hospital stays are shorter for patients who’ve received monoclonal antibodies – four days, as compared to nearly seven for all COVID-positive patients.
“What we’ve found is that monoclonal antibody therapy, when administered at the right time, really works,” said Dr. Cynthia Maree, infectious disease specialist for St. Charles. “It’s the only outpatient treatment we have for COVID right now, but the good news is that it limits the severity of illness, keeps people out of the hospital and helps them feel better faster.”
To be clear, Maree said, MAB therapy should not be considered an alternative to vaccination. Getting vaccinated is still the best way to protect yourself and others against COVID-19, she said.
Cornelius is walking, talking proof that pursuing the treatment can make a difference. The day she learned she qualified for MAB therapy, she started having trouble breathing and her heart began pounding, she said.
“That’s when I realized, ‘Wow, this is how people die of COVID,’” she said. “I was really struggling that night and just felt so glad that I was vaccinated and that I had this treatment on the horizon.”
The next day, Cornelius spoke with her primary care physician, who referred her to St. Charles. (Patients cannot self-refer for MAB therapy. They must be referred by a physician.) And then one day later, she went to St. Charles Redmond to receive the infusion. Generally speaking, the treatment takes a couple of hours, including time after the infusion for observation and recovery.
Cornelius received her infusion on a Thursday evening. By Saturday, she said, she was feeling much better.
“If you didn’t know I’d had it, you wouldn’t have been able to tell,” she said. “And then on Sunday and Monday, my senses of taste and smell came back.”
Cornelius credits monoclonal antibody therapy – along with “therapeutic doses” of vitamins and elderberry, she said – with “getting (her) over the hump” and on the road back from COVID-19.
“I 100% think it boosts your recovery,” she said. “I don’t even want to think about what might’ve happened had I not seen that MyChart note and talked to my doctor about it. That one bad night I had was scary, and you see so many stories about people who think they’re getting better and then suddenly, they take a turn for the worse.”
With the Delta variant spreading rapidly in Central Oregon and more people contracting the virus every day, Cornelius has a simple message: “If you do test positive, don’t assume that you don’t qualify,” she said. “Ask your doctor and find out because it’s going to help you get better.”
Learn more about monoclonal antibody therapy at St. Charles.